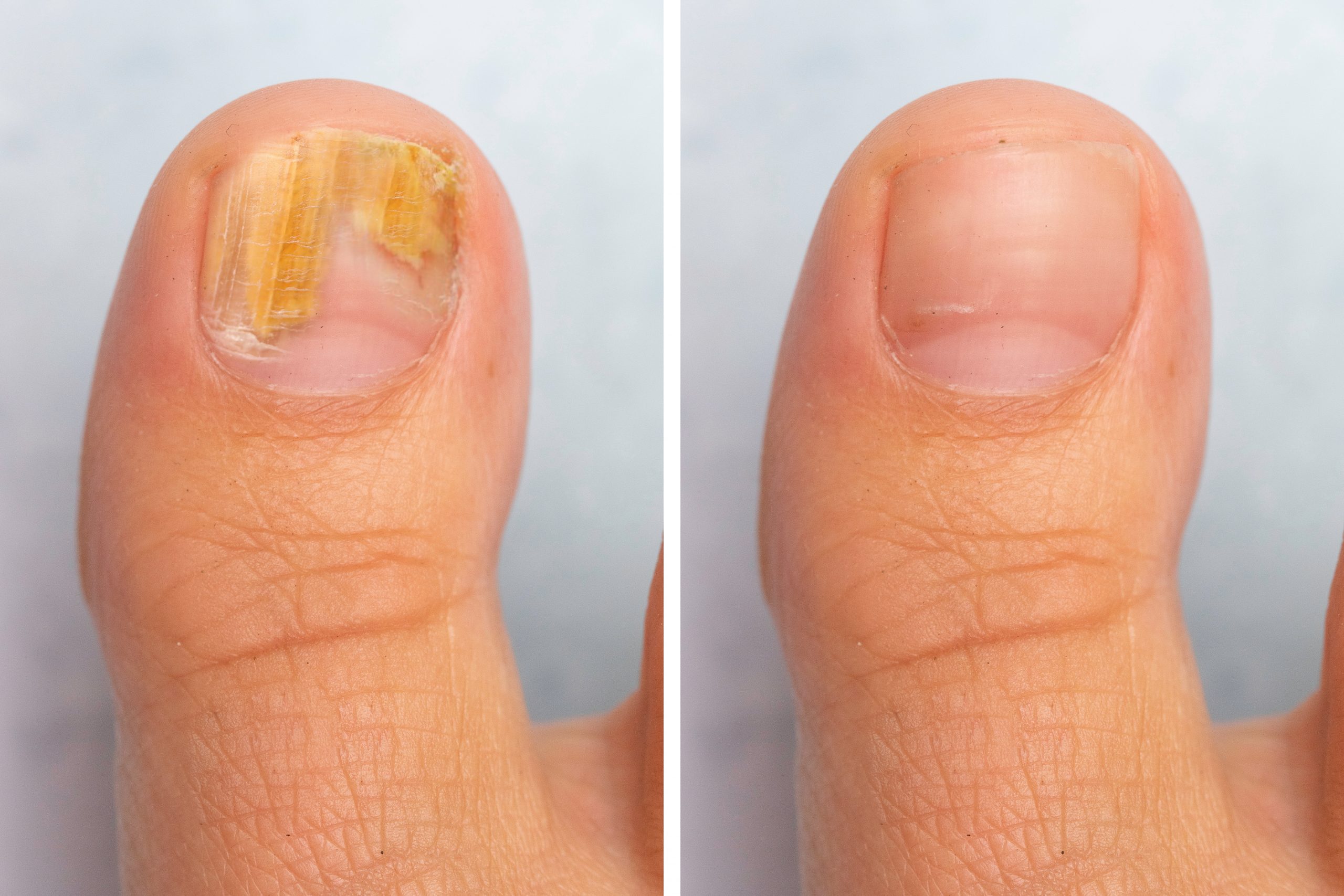
Toenail fungus, medically known as onychomycosis, is a common condition that affects many individuals. However, people with diabetes are at a higher risk of developing toenail fungus due to the potential impact of diabetes on foot health. Understanding the connection between toenail fungus and diabetes is crucial for individuals with diabetes to maintain optimal foot health. In this article, we will explore the link between toenail fungus and diabetes and discuss strategies for prevention and management.
- Weakened Immune System: Diabetes can weaken the immune system, making individuals more susceptible to infections, including toenail fungus. Elevated blood sugar levels can impair the body’s ability to fight off fungal infections, allowing fungi to thrive and invade the toenails. People with diabetes should be vigilant about foot hygiene and take extra precautions to minimize the risk of developing toenail fungus.
- Circulatory Issues: Diabetes can lead to circulatory problems, including reduced blood flow to the extremities, including the feet. Poor circulation can impair the delivery of essential nutrients and immune cells to the toenails, making them more susceptible to infections. Reduced blood flow also hampers the body’s ability to combat fungal infections effectively. Maintaining good blood sugar control and practicing foot care routines can help mitigate the impact of circulatory issues on toenail health.
- Nerve Damage: Peripheral neuropathy is a common complication of diabetes, characterized by nerve damage that can lead to reduced sensation in the feet. Individuals with neuropathy may not notice early signs of toenail fungus, such as discoloration or thickening of the nails. Without prompt treatment, the infection can worsen and lead to more severe complications. Regular foot examinations by healthcare providers and self-monitoring are essential for individuals with diabetes to detect toenail fungus early.
- Foot Care Practices: Proper foot care is crucial for individuals with diabetes to prevent and manage toenail fungus. It is essential to keep the feet clean and dry, paying special attention to the areas between the toes. Regularly inspecting the toenails for any changes, such as discoloration or brittleness, can help detect toenail fungus at an early stage. Trimming nails straight across and avoiding tight-fitting shoes can minimize the risk of toenail injuries that may facilitate fungal infections.
- Prompt Treatment: Timely treatment is essential for managing toenail fungus in individuals with diabetes. Due to the potential complications associated with diabetes, such as impaired wound healing and increased susceptibility to infections, professional medical advice should be sought for proper diagnosis and treatment. Treatment options may include topical antifungal medications, oral antifungal drugs, or a combination of both. Your healthcare provider can recommend the most suitable treatment based on your specific condition.
- Comprehensive Foot Care: Managing toenail fungus in individuals with diabetes requires a comprehensive approach to foot care. This includes regular visits to a podiatrist or foot specialist, who can provide guidance on proper nail care and recommend appropriate treatment options. It is crucial to maintain good blood sugar control, as elevated blood sugar levels can exacerbate toenail fungus and hinder the healing process.
- Prevention Strategies: Prevention is key when it comes to managing toenail fungus in individuals with diabetes. Some preventive measures include wearing breathable footwear, avoiding walking barefoot in public places, keeping feet dry and clean, wearing moisture-wicking socks, and using antifungal powders or sprays when necessary. Additionally, practicing good diabetes management, such as monitoring blood sugar levels, following a healthy diet, and engaging in regular physical activity, can support overall foot health.
- Collaborative Care: Managing toenail fungus in individuals with diabetes requires collaboration between healthcare providers, including primary care physicians, endocrinologists, pod