For individuals with diabetes, managing blood sugar levels is crucial for overall health and well-being. One hormone that plays a central role in this process is insulin. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels and allows cells to utilize glucose for energy. In this article, we will explore the essential role of insulin in managing blood sugar levels and its significance for individuals with diabetes.
- Glucose Regulation: Insulin acts as a key regulator of glucose in the body. When we consume carbohydrates, they are broken down into glucose, which enters the bloodstream. In response, the pancreas releases insulin to signal cells to take up glucose from the bloodstream. Insulin helps to transport glucose into cells, where it can be used for energy production or stored for later use.
- Facilitates Cellular Uptake: Insulin binds to specific receptors on the cell surface, initiating a series of signaling events that allow glucose to enter the cell. It promotes the transport of glucose from the bloodstream into muscle, fat, and liver cells. Without insulin, glucose remains in the bloodstream, leading to high blood sugar levels.
- Storage of Excess Glucose: Insulin plays a vital role in storing excess glucose for future use. When blood sugar levels are high, such as after a meal, insulin signals the liver and muscle cells to store glucose as glycogen. This stored glycogen can be released when blood sugar levels drop, providing a steady supply of glucose between meals or during periods of fasting.
- Inhibits Gluconeogenesis: Gluconeogenesis is the process of glucose production in the liver from non-carbohydrate sources, such as proteins or fats. Insulin helps to suppress this process, ensuring that blood sugar levels do not rise excessively. By inhibiting gluconeogenesis, insulin helps to maintain stable blood sugar levels.
- Modulates Fat Metabolism: Insulin also plays a role in fat metabolism. It promotes the synthesis of fatty acids in the liver, which are then stored as triglycerides in adipose tissue. In the presence of insulin, fat cells take up and store fatty acids, preventing the release of excessive amounts of fatty acids into the bloodstream. This action helps to regulate lipid metabolism and prevent the development of conditions like hyperlipidemia.
- Counteracts the Effects of Counterregulatory Hormones: Counterregulatory hormones, such as glucagon and cortisol, work to raise blood sugar levels. Insulin counteracts these hormones, inhibiting their effects and helping to maintain blood sugar within a healthy range. This balance between insulin and counterregulatory hormones is critical for blood sugar control.
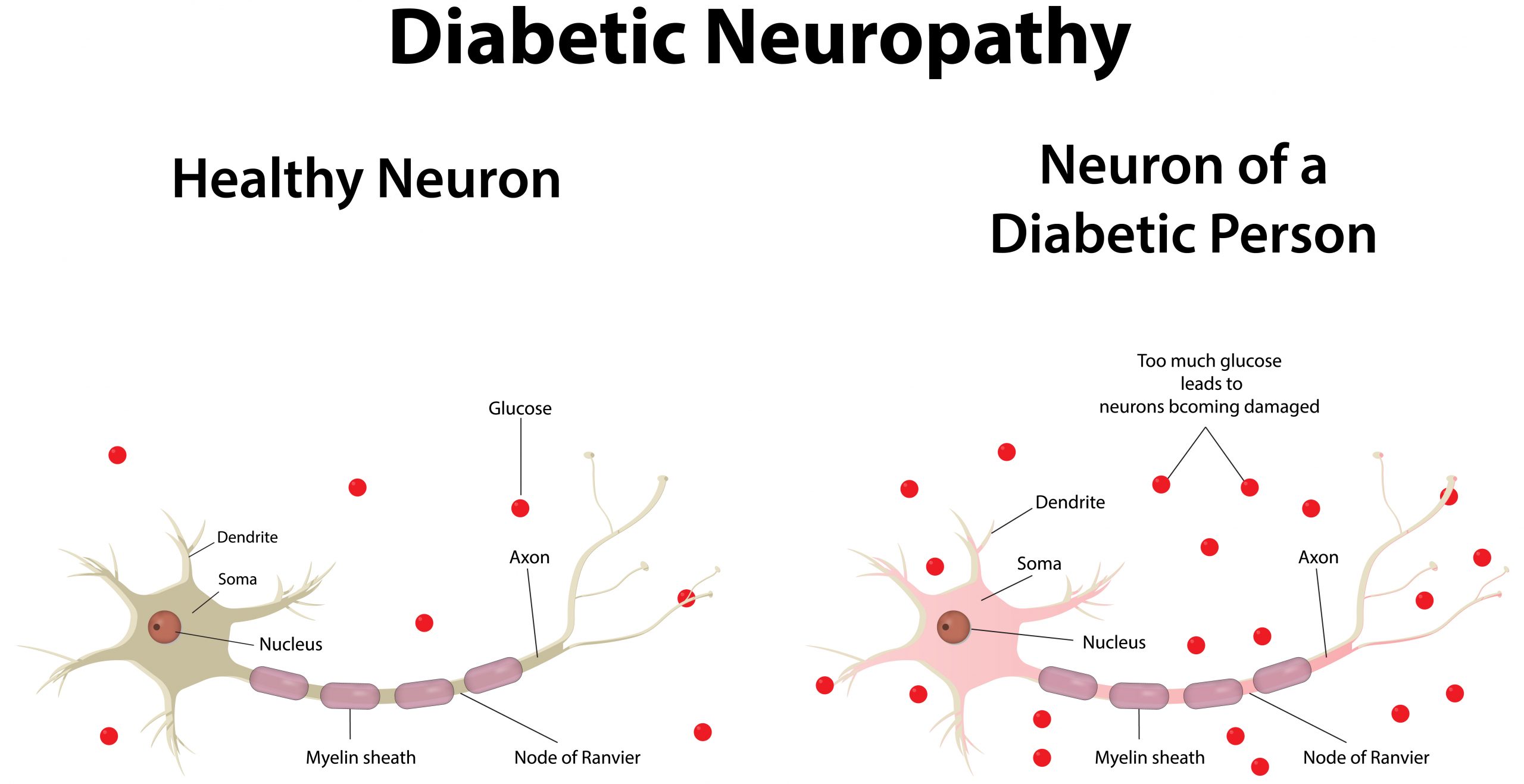
- Impaired Insulin Function in Diabetes: In individuals with diabetes, the production or effectiveness of insulin is compromised. In type 1 diabetes, the immune system mistakenly attacks and destroys insulin-producing cells in the pancreas, resulting in a lack of insulin production. In type 2 diabetes, the body becomes resistant to the effects of insulin, leading to elevated blood sugar levels. In both cases, managing blood sugar levels involves administering insulin (in type 1 diabetes) or improving insulin sensitivity (in type 2 diabetes).
- Importance of Insulin Therapy: For individuals with type 1 diabetes, insulin therapy is necessary to maintain blood sugar control. Insulin can be administered through injections or insulin pumps, mimicking the natural release of insulin by the pancreas. In type 2 diabetes, insulin therapy may also be prescribed when other treatment modalities, such as oral medications or lifestyle changes, are insufficient to manage blood sugar levels.
In conclusion, insulin plays a vital role in managing blood sugar levels. It facilitates the uptake of glucose into cells, regulates glucose